
Elisa Black moved back home when she was 25 years old because she couldn’t cope on her own. She locked herself in her room for three months, convinced she would die if she left her house.
Already nervous as a child, Elisa had developed obsessions early in life about gaping mud puddles that might swallow her parents. As she grew up, she developed new phobias: fear of germs, fear of getting leprosy, fear of water, fear of eating in public because she might vomit. She was plagued by panic attacks. There was always “the eternal feeling that something catastrophic was about to happen” – a feeling of anxiety that all of us may have sometimes, but for some, like Elisa, are ever-present and dominating.
Elisa tried many things to treat her anxiety. She visited psychiatrists and took loads of medications: Aropax, Cipramil, Effexor, Zoloft. She saw psychologists and tried cognitive behavioural therapy (CBT), hypnosis and exposure therapy, before going on to experiment with yoga, exercise, meditation, naturopathy, herbal therapy and more.
Finally, after years of failing and even blaming herself for not trying hard enough, she stumbled onto something that finally worked. That something was B vitamins.
Elisa recounts her story in The Anxiety Book: A True Story of Phobias, Flashbacks and Freak-Outs and How I Got My Inner Calm Back (Hachette Australia, 2016). But hers is only one of thousands of cases of people who are now turning to a ‘micronutrient’ approach to mental health and finding a permanent solution without the harm of psychotropic drugs.
One name, many faces
Anxiety is one of the more common psychiatric illnesses, affecting around 18 per cent of Americans,1 and more than eight million Brits.2
Anxiety disorders affect women more than men and encompass a host of diagnostic labels, including panic disorder, social anxiety disorder, generalized anxiety disorder, post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD). They are frequently disabling and cost people socially, personally and professionally. In the US alone, their economic impact was estimated as nearly $47 billion – almost a third of the costs of all mental disorders.1 Bad enough to cope with on its own, anxiety frequently morphs into other ‘mood disorders’ like depression and bipolar disorder, with its swings from manic ‘highs’ of uncontrolled and often misdirected energy to depressive ‘lows’ of gloomy despair and inactivity.
Notoriously unsuccessful
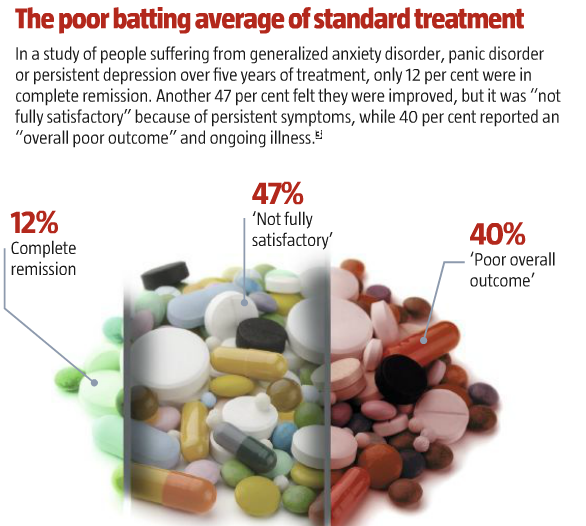
The medical literature admits that anxiety is “notoriously difficult to successfully treat” and estimates that at least a third of patients do not respond to the standard treatments.1 But that may be a generous estimate. Several studies of anxiety treatment put the failure rate much higher. One, for example, looked at people suffering from generalized anxiety disorder, panic disorder or persistent depression over five years of treatment, and found that only 12 per cent were in complete remission. Another 47 per cent felt they were improved, but it was “not fully satisfactory” because of persistent symptoms, while 40 per cent reported an “overall poor outcome” and ongoing illness.3
“Despite notable advances, many patients with anxiety disorders fail to adequately respond to existing pharmacologic treatments,” concluded one overview of the anxiety treatment landscape in a resounding understatement.4
Drug dangers
Nor have advances within medicine been radical. For more than 50 years, doctors have doled out tranquillizers, usually benzodiazepines like Valium and Xanax. As the evidence for their strong potential for addiction became overwhelming – with horrendous, well-documented withdrawal symptoms, as well as brain damage and a 50 per cent risk of Alzheimer’s disease5 – their use as a first-line approach is finally being discouraged.
For decades now, the starter treatment for anxiety has shifted to antidepressants, serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, while the second line of treatment comprises different categories of antidepressants: tricyclic antidepressants and monoamine oxidase inhibitors. For ‘resistant’ cases, doctors may try antipsychotics like Risperdal or Abilify. However, besides their lack of effectiveness, these psychotropic drugs are all associated with known side-effects that frequently make patients feel so nauseated or ‘zoned out’ that they soon become unwilling to continue taking them.
Worse, a major study involving repeated brain scans over up to 14 years confirmed what many had suspected: antipsychotic drugs cause brain damage by progressively reducing brain tissue volume, leading to cognitive impairment.6
This class of drugs is also linked to a raft of other health problems, including obesity, high blood pressure, diabetes and tardive dyskinesia (a neurological disorder with involuntary and uncontrollable movements, or tics), slurred speech, tremors, anxiety, inability to sit still, inner restlessness, distress and paranoia – hardly the ‘cure’ anxiety sufferers are looking for.
Orthomolecular approach
“Drugs make a well person sick. How can drugs make a sick person well?” was the simple question posed by the late Abram Hoffer, the Canadian psychiatrist who became interested in the nutritional treatment of mental disorders. He was among the first to see the similarities between symptoms of schizophrenia and those of vitamin B3 (niacin) deficiency, or pellagra: mental confusion and dementia.
“If vitamin B-3 (nicotinic acid and/or nicotinamide) were removed from our food, we would all become psychotic within one year,” Hoffer wrote. “Long before the psychosis appeared, there would be an equally widespread pandemic of neuroses in all its forms – depression, hypochondriasis, anxiety, and obsessive compulsive states, and personality deviations.”7
In the 1950s, Hoffer began to treat tens of thousands of schizophrenics with diets free of sugar and highly refined carbohydrates, plus megadoses of vitamin B3 and sometimes vitamin B6, reportedly with “astonishing” success.8
Because vitamins and minerals are involved in virtually every biological process, micronutrient deficiencies tend to scatter symptoms throughout the body. B vitamins play an essential role in cellular metabolism, and are necessary in adequate supply to provide energy for the body and brain.
It makes sense that things go wrong if they’re lacking. In fact, all the recognized symptoms of deficiencies of the various B vitamins have been linked to disorders of the nervous system.
Mainstream medicine and psychiatry maintain that our diet supplies more than enough of these nutrients and that deficiencies are rare, but many people disagree. As Charles Popper, a Harvard psychiatrist, says, “Micronutrient insufficiencies affect most people, even in ‘well-fed’ populations, especially patients with psychiatric disorders, including mood disorders in youth and adults.”
According to Popper, modern agricultural techniques, loss of nutrients from the soil, food-processing, and the widespread consumption of highly processed junk foods and sugars all block absorption of or create increasing demand for these nutrients, and he claims these factors have all contributed to the rise in mental illnesses.9
MTHFR gene mutations
There is inc reasing evidence that a genetic mutation of the MTHFR gene, which provides instructions for making an important enzyme called methylenetetrahydrofolate reductase (MTHFR), can leave as many as one in five people with difficulty processing B-group vitamins. This inability, which leads to deficiencies of these nutrients, has been linked to everything from anxiety and depression to multiple miscarriages, stroke, cardiovascular disease and diabetes, among many other illnesses.
Elisa Black tested positive for this gene mutation. When her doctor prescribed a version of folate called ‘folinic acid’ and a version of vitamin B12 known as ‘methyl B12’ (methylcobalamin, a more readily bioavailable form of the vitamin that supports body metabolism), the results for her were life-changing. “If only I’d known that something as simple – and free of side-effects – as B vitamins were a credible option before I spent all my money on enough hand sanitizer to keep all the world’s bacteria at bay,” she says.
The average GP, however, is a long way from either understanding MTHFR mutations or appreciating their possible links with mental conditions. “Most medical professionals will disagree there is a link with anxiety or depression,” naturopath Carolyn Ledowsky, founder of MTHFR Support Australia, told Black, “but 70 per cent of our MTHFR patients present with anxiety.”
“Most MTHFR patients with anxiety also have decreased B6 and zinc in the body,” Ledowsky adds. “When this is addressed and B12 and folate levels are restored, anxiety will be decreased by about 80 per cent within three weeks or so.”
Functional physician Jill Carnahan recommends that patients get a 23andme DNA test to determine whether they are carriers of an MTHFR gene variant, and advises increased supplementation if they test positive. “Make sure you supplement with essential nutrients, like methyl B12, methylfolate, trimethylglycine (TMG), N-acetylcysteine, riboflavin, curcumin, fish oil, vitamins C, D and E, and probiotics” (see box, right).
But it’s a tricky balance, adds Carnahan, because people who have inherited MTHFR mutations in both copies of the gene should proceed very cautiously with methyl B12 and methylfolate supplementation, as they may not be able to process high doses. “And use extreme caution when supplementing with niacin, which can dampen methylation.”10
“Overall, there is sufficient evidence to support at least the use of high-dose B vitamins in the treatment of stress and anxiety in the general population, with one study suggesting even greater benefit when B vitamins are combined with a broad array of minerals,” writes Julia Rucklidge, professor of psychology at the University of Canterbury, and Bonnie Kaplan, professor of community health sciences at the University of Calgary in Alberta, Canada, in a recent review of the scientific literature.11 Increasingly researchers favour the use of “broad spectrum” vitamins and minerals, rather than megadoses of single nutrients like niacin or vitamin B12.
Rucklidge and Kaplan have conducted studies on a branded multivitamin called EMPowerplus from a company called Truehope, founded by Alberta father Tony Stephan, whose wife Debbie suffered from bipolar disorder and committed suicide in 1994. He was desperate for help when his teenage son, Joseph, and his adult daughter, Autumn, were also diagnosed as bipolar, as both were taking lots of medications and considered at high risk of suicide.
The doctors had told Stephan there was no hope for his children and to “accept reality” and prepare for the worst. Then, during a chance discussion with a friend, David Hardy, who made livestock feed for farmers, Stephan noticed similarities in the symptoms of mental illness in humans and certain behaviours in pigs. It was commonplace to treat irritable penned hogs with nutrition, and Hardy had found particular success with certain vitamins and trace minerals.
The pair set up a makeshift lab in a kitchen and created a human version of Hardy’s pig feed by combining four different products with numerous other ingredients, which they tried out on Stephan’s son, Joseph. After five days on the supplement, Joseph was completely turned around. “All of a sudden he became gentle,” recalls his father. “His demeanour changed. He was starting to think positively about his life.”
Meanwhile, Stephan’s daughter Autumn was on suicide watch after having been given a load of psychotropic drugs for paranoia and panic disorders; she was also not allowed to be with her baby alone because of her homicidal thoughts. Five days after being given the revised pig formula, she turned her first corner. She was able to take her first shower without keeping her clothes on for fear of being attacked. She continued to improve and, over the next few years, she recovered completely.
Amazed by their results, Stephan and Hardy took their product to interested researchers and academics. As a result, their 36-ingredient current formula, known as EMPowerplus, has become one of the most tested multivitamin formulations for mental health.
This is all the more unusual as any such research has been thwarted for decades by the conventional emphasis on psychiatric solutions for mental health issues, and also because there’s far less profit to be made from natural substances than from drugs.
Rucklidge and Kaplan conducted controlled surveys of levels of anxiety and PTSD in people after the 2010-2011 earthquake in Christchurch, New Zealand, and after floods in Calgary: just four to six weeks of EMPowerplus significantly (and even “very much” )improved mood, anxiety and energy.12
Two case studies – an 11-year-old boy with psychosis and OCD, and a 12-year-old boy with bipolar disorder – both confirmed that this micronutrient treatment was “superior to conventional treatment”, with improvements that were reversed when the supplement was stopped.13
Rucklidge is now studying the effects of a related formula from David Hardy’s company, Hardy
Nutritionals, in pregnant women. Both the original formula and the formula for pregnancy differ widely from the standard vitamin preparations found on supermarket shelves, says Rucklidge, as they have higher doses of brain-related vitamins and a broader array of trace minerals (see box, above).
The stories of people’s recoveries from anxiety and mood disorders using supplements continue to grow. Gloria Steinlein had been unable to work or take care of herself because she was plagued with anxiety and panic attacks and was repeatedly hospitalized – before she started taking EMPowerplus.
“That big gaping empty hole that I had inside of me when I was ill, that unrelenting pain that would just never let up and it felt like it was darkness all the time,” she says, “to have that gone and to have that replaced by happiness every day is unbelievable.”
Vitamins and the brain
Two-time Nobel Prize winner and molecular biologist Linus Pauling, who championed the use of high-dose vitamin C for numerous medical issues, was fascinated by psychiatrist Abram Hoffer’s work. In 1968, Pauling coined the term ‘orthomolecular’ to describe the practice of preventing and treating disease by providing the body with optimal amounts of natural substances, including vitamins. This new category of medicine included ‘orthomolecular psychiatry’, as practised by Hoffer.
There has never been a diagnostic test to demonstrate that any psychiatric illness, including anxiety, results from a chemical imbalance, but the studies that have investigated the nutritional status of psychiatric patients have noted that such people are usually deficient in certain B vitamins and minerals.1
More recently, a Turkish study of 52 children and adolescents suffering from OCD showed significantly lower levels of vitamin B12 and vitamin D, and higher levels of homocysteine, compared with 30 healthy controls.2 MTHFR gene mutations (see main article) also affect processing of this amino acid. In fact, elevated levels of homocysteine appear to have a causal relationship with schizophrenia,3 and increase the risk of dementia and Alzheimer’s disease.4
Natural cures for anxiety
The following have all shown evidence of effectiveness for a variety of anxiety issues.
Eat fish, fish oils and flaxseed. Dietary deficiency of docosahexaenoic acid (DHA), a component of fish oil (omega-3 fatty acid), has long been associated with an increased risk of anxiety disorders. Essential fatty acids can alleviate prenatal stress, cortisol levels, and both premenstrual and menopausal anxiety in women.1
Suggested daily dosage: You can purchase high-dose or pure DHA fish oil, flaxseed or flaxseed oil. Aim for 20 g/day or more of both DHA and eicosapentaenoic acid (EPA)
Take magnesium. Animal studies link magnesium deficiency with anxiety,2 whereas combining magnesium with vitamin B6 may reduce premenstrual syndrome anxiety and mild anxiety in women.3
Suggested daily dosage: Magnesium oxide: 200-600 mg; vitamin B6 (pyridoxine): 50 mg
Add vitamin C. High-dose sustained-release vitamin C may reduce anxiety and mitigate increased blood pressure in response to stress.1
Suggested daily dosage: 8 g (in separated doses of 2-g each)
Spice it up. Curcumin, a component of the spice turmeric found in Indian food or as a supplement, has been demonstrated to enhance DHA synthesis, particularly when from the vegan source of linseed oil.4
Suggested daily dosage: 500 mg of curcumin twice a day (as capsules)
Feed your gut bugs. Eating more prebiotics may help to undo the damage caused by stress by feeding and nurturing ‘good’ gut bacteria. Prebiotics are found in plant fibre, such as raw chicory root, raw Jerusalem artichokes, raw dandelion greens, raw garlic, raw leeks, raw asparagus, and raw and cooked onions. Preliminary lab studies suggest that prebiotics may also help safeguard good bacteria during stressful times, say researchers from the University of Colorado, and might even help re-establish good sleeping patterns which, in turn, can also offset anxiety.5
Probiotics, which include yoghurt, kefir (see page 49) and fermented vegetables like sauerkraut, introduce good bacteria back into the gut.
Get moving. Texas researchers reviewing dozens of studies discovered that exercise affects areas of the brain that can counteract depression and anxiety. Improvements in mood and stress levels can be seen after just 25 minutes of exercise.6
Suggested daily dosage: 2-2.5 hours of moderate to high-intensity exercise a week
Look to herbs. Kava (Piper methysticum) has been shown to dramatically reduce anxiety, especially in more severe cases, after just six weeks, with no adverse reactions or dependency issues in a University of Melbourne sutdy.7
Extracts of St John’s wort (Hypericum perforatum), long used in traditional medicine and licensed in Germany to treat anxiety, depression and sleep disorders,8 have been shown to be as effective as antidepressant drugs, with far fewer side effects. They increase numbers of serotonin receptors, which may be the key to depression, rather than levels of serotonin itself.
Suggested daily dosage: 120 mg of kava twice a day, 300-1,000 mg of St John’s wort
What’s in the supplements that work?
A few different formulas in easy-to-swallow capsules or powders to mix into drinks have evolved from Hardy’s original formula, including Hardy’s Daily Essential Nutrients, and from Truehope’s EMPowerplus Methylated Advanced original formula of 36 nutrients.
Both suggest daily servings containing:
• B12 at levels of 240-1200 mcg (far more than the 2.4 mcg recommended by mainstream dietitians)
• high methylfolate contents of 384-1068 mcg
• thiamine (B3) levels of 4.8-80 mg
• niacin at levels of 24-120 mg (modest compared with orthomolecular recommendations of 100-600 mg three times a day)
• vitamin D at 384-4,000 IU
• additional levels of vitamins A, C and E, plus zinc, magnesium, molybdenum, selenium and chromium – all essential for nervous system function.
• trace amounts of lithium orotate (IN Hardy’s formula only), found to help people with depression, anxiety and obsessive-compulsive disorder (OCD).1§
< p class="FeatBoxoutEdsALT">Vitamins and the brain
|
References |
|
|
1 |
Prostaglandins Leukot Essent Fatty Acids, 2006; 74: 75-85; Am J Psychiatry, 2004; 161: 1705-8 |
|
2 |
Psychiatry Res, 2017; 254: 232-7 |
|
3 |
BMC Med Genet, 2015; 16: 54 |
|
4 |
Brain, 2013; 136: 2707-16 |
Natural cures for anxiety
|
References |
|
|
1 |
JBI Database System Rev Implement Rep, 2017; 15: 402-53 |
|
2 |
Neuropharmacology, 2012; 62: 304-12 |
|
3 |
Nutrients, 2017; 9: 429; doi: 10.3390/nu9050429 |
|
4 |
Biochim Biophys Acta, 2015; 1852: 951-61 |
|
5 |
Front Behav Neurosci, 2017; 10: 240; doi: 10.3389/fnbeh.2016.00240 |
|
6 |
Front Psychiatry, 2013; 4: 27; doi: 10.3389/fpsyt.2013.00027 |
|
7 |
J Clin Psychopharmacol, 2013; 33: 643-8 |
|
8 |
BMJ, 1996; 313: 253-8 |
What’s in the supplements that work?
|
References |
|
|
1 |
Nutr J, 2008; 7: 2 |
Main article
|
1 |
Dialogues Clin Neurosci, 2015; 17: 305-17 |
|
2 |
www.mentalhealth.org.uk/statistics/mental-health-statistics-anxiety |
|
3 |
Psychol Med, 1998; 28: 1149-57 |
|
4 |
J Clin Psychiatry, 2010; 71: 839-54 |
|
5 |
BMJ, 2014; 349: g5205 |
|
6 |
Arch Gen Psychiatry, 2011; 68: 128-37 |
|
7 |
Psychosomatics, 1970; 11: 522-5 |
|
8 |
Can Fam Physician, 1975; 21: 78-82 |
|
9 |
Child Adolesc Psychiatr Clin N Am, 2014; 23: ix-xii |
|
10 |
http://doccarnahan.blogspot.co.uk/2013/05/mthfr-gene-mutation-whats-big-deal.html |
|
11 |
Expert Rev Neurother, 2013; 13: 49-73 |
|
12 |
Hum Psychopharmacol, 2012; 27: 440-54; Psychiatry Res, 2015; 228: 373-9 |
|
13 |
BMJ Case Rep, 2012; doi: 10.1136/bcr-2012-007213; J Child Adolesc Psychopharmacol, 2009; 19: 453-60 |
What do you think? Start a conversation over on the... WDDTY Community